SOMATIC CELL THERAPY MEDICAL PRODUCTS (sCTMPs)
General
sCTMPs contain cells or tissues that have been manipulated to change their biological characteristics or cells or tissues not intended to be used for the same essential functions in the body. They can be used to cure, diagnose or prevent diseases;
An sCTMP has the following characteristics:
- It contains or consists of cells or tissues that have been subject to substantial manipulation so that biological characteristics, physiological functions or structural properties relevant for the intended clinical use have been altered; or it contains or consists of cells or tissues that are not intended to be used for the same essential function(s) in the recipient as in the donor.
- It is presented as having properties for, or is used in or administered to, human beings with a view to treating, preventing or diagnosing a disease through the pharmacological, immunological or metabolic action of its cells or tissues.
The EMAs scientific guidelines on cell therapy and tissue engineering help medicine developers prepare marketing authorisation applications for human medicines, where clinical trial documentation plays a crucial role. Multidisciplinary: cell therapy and tissue engineering
Quality (including manufacturing)
Selected guidelines regarding sCTMPs, focusing on quality:
- Human cell-based medicinal products: Guideline CHMP/410869/06(PDF)
- On potency testing of cell-based immunotherapy medicinal products for the treatment of cancer: Guideline EMA/CHMP/BWP/271475/2006 rev. 1(PDF)
- Risk-based approach according to Annex I, part IV of Directive 2001/83/EC applied to ATMPs: Guideline CAT/CPWP/686637/2011(PDF)
- Creutzfeldt-Jakob disease and advanced therapy medicinal products: Position statement EMA/CHMP/CAT/BWP/353632/2010(PDF)
For more specific applications, see the following documents:
- Xenogeneic cell-based medicinal products: Guideline CHMP/CPWP/83508/09(PDF)
- In-vitro cultured chondrocyte containing products for cartilage repair of the knee: Reflection paper CAT/CPWP/568181/2009(PDF)
- Stem cell-based medicinal products: Reflection paper EMA/CAT/571134/2009(PDF)
Non-clinical (pre-clinical)
Non-clinical studies are designed to support the use of a specific product to treat a specific clinical indication.The non-clinical studies conducted are an important element of the overall development pathway for an IMP and significant for establishing feasibility and reasonable safety of the IMP’s proposed clinical route of administration. The overall objectives for a sufficient non-clinical programme for an sCTMP may include:
- Establishing biological plausibility
- Identifying biologically active dose levels
- Selecting the potential starting dose level, dose-escalation schedule and dosing regimen for clinical trials
- Establishing feasibility and reasonable safety of the investigational product’s proposed clinical route of administration
- Supporting patient eligibility criteria
- Identifying physiological parameters which can guide clinical monitoring
- Identifying potential public health risks (e.g. to the general public, caregivers, family members, close contacts (for example co-workers) and intimate contacts)
The resulting data from pre-clinical studies should address these objectives in order to guide the design of early-phase clinical trials, as well as to establish a platform for the conduct of future pre-clinical studies that may be needed to support later phases of product development.
Non-clinical studies using cell-based medicinal products should be performed in relevant species. Considering the nature of these products this is specifically challenging. It is always recommended to seek the advice of the relevant authorities when selecting the species for non-clinical studies, especially pivotal safety studies. Homologous products could be used, however in such cases bridging data to the human product is of the utmost importance.
ATMPs and cell-based ATMPs in particular present additional challenges that should be addressed, such as:
- Cell survival status following delivery
- Cell migration or trafficking to non-target sites
- Cell differentiation into undesired cell types
- Development of an immune response to the cells
- Uncontrolled proliferation or tumorigenicity
The EMA has a set of scientific guidelines on the non-clinical testing of a medicinal product; these guidelines are provided for:
- Environmental risk assessment
- Non-clinical development
- Pharmacology and safety pharmacology
- Toxicology
ATMPs differ from traditional medicinal products and some aspects of the guidelines may not be applicable. However, in such cases a rationale and risk assessment for not following the guidelines shall be available.
IMPORTANT LINK:
Setting standards of quality and safety for the collection, testing, processing, storage and distribution of human blood and blood components and amending Directive 2001/83/EC, Directive2002/98/EC.
Clinical
FIRST-IN-HUMAN
When the IMP is being tested for the first time in humans, it is useful to read the following guidelines from the EMA:
- Strategies to identify and mitigate risks for first-in-human and early clinical trials with investigational medicinal products(PDF)
- Guideline on requirements for first-in-human clinical trials for potential high-risk medicinal products
PHASE I/II TRIAL OBJECTIVES
The main purpose of a Phase I/II trial is safety evaluation; this includes assessment of the nature and frequency of potential adverse reactions and an estimation of the relationship to dose, but also other issues, such as feasibility of administration and pharmacological activity.
Since the sCTMP candidate may in fact have little or no toxicity, it may not be worthwhile using toxicity as an endpoint. Biological outcomes, such as engraftment, gene expression, optimal biological dose or immune response to a vaccine are alternatives for primary endpoints. Secondary objectives for efficacy measures, either short-term response or longer-term outcomes, should be included for support in the design of later-phase trials.
FEASIBILITY ASSESSMENTS
Feasibility assessments are carried out if specialised devices or novel procedures are required for administration, customised preparation of products, special handling of products (e.g. very short expiration time) or adjunctive therapy. Consideration should be given to designing early-phase trials to identify and characterise any technical or logistical issues in the manufacturing or administration of the product. Such issues may need to be addressed before proceeding with further product development.
DOSE EXPLORATION
When using cell therapies for life-threatening diseases, some toxicities may be expected and acceptable. In these situations, the main objective might be to identify the maximum tolerated dose (MTD), i.e. the highest dose that can be given with acceptable toxicity using a dose-escalation protocol.
For some cell therapies, toxicity is not expected to be substantial in the predicted therapeutic range. In this situation, the objective of dose exploration may be to determine the range of biologically active or optimal effective doses.
In some cases, indicators of potential benefit may plateau above a certain dose such that further dose escalation to reach a maximum tolerated dose may be unnecessary.
ACTIVITY ASSESSMENTS
Potential efficacy could be indicated by any of the following short-term responses and longer-term outcomes:
- cell engraftment
- morphologic alterations
- more common measures such as changes in immune function
- tumour shrinkage
- physiological responses to various assessments
PHASE III TRIAL OBJECTIVES
Phase III usually is considered to begin with the initiation of studies in which the primary objective is to demonstrate or confirm therapeutic benefit. Studies in Phase III are designed to confirm the preliminary evidence accumulated in Phase II that a drug is safe and effective for use in the intended indication and recipient population.
These studies are intended to provide an adequate basis for marketing approval.
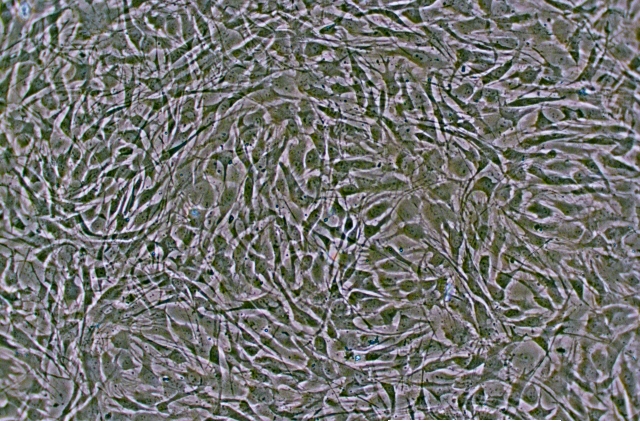
Photo by: Cell and Tissue Laboratory, Sahlgrenska University Hospital
