TISSUE ENGINEERED PRODUCTS (TEPs)
General
TEPs contain cells or tissues that have been modified so they can be used to repair, regenerate or replace human tissue.
A TEP has the following characteristics:
- It contains or consists of cells or tissues that have been subject to substantial manipulation so that biological characteristics, physiological functions or structural properties relevant for the intended clinical use have been altered; or it contains or consists of cells or tissues that are not intended to be used for the same essential function(s) in the recipient as in the donor.
- It is presented as having properties for, or is used in or administered to, human beings with a view to regenerating, repairing or replacing a human tissue.
Quality (including manufacturing)
Selected guidelines regarding TEPs, focusing on quality:
- Human cell-based medicinal products: Guideline EMEA/CHMP/410869/2006
- Certain technical requirements for the coding of human tissues and cells:Directive2015/565/EC
Non-clinical (pre-clinical)
Non-clinical studies are designed to support the use of a specific product to treat a specific clinical indication.The non-clinical studies conducted are an important element of the overall development pathway for an investigational product. They facilitate the establishment of feasibility and reasonable safety (case-by-case according to risk assessment) of the investigational product’s proposed clinical route of administration. The overall objectives for a sufficient pre-clinical programme for a TEP may include:
- Establishing biological plausibility
- Identifying biologically active dose levels
- Selecting the potential starting dose level, dose-escalation schedule and dosing regimen for clinical trials
- Establishing feasibility and reasonable safety of the investigational product’s proposed clinical route of administration (ROA)
- Supporting patient eligibility criteria
- Identifying physiological parameters which can guide clinical monitoring
- Identifying potential public health risks (e.g. to the general public, caregivers, family members, close contacts (for example co-workers) and intimate contacts)
The resulting data from pre-clinical studies should address these objectives in order to guide the design of early-phase clinical trials, as well as to establish a platform for the conduct of future pre-clinical studies that may be needed to support later phases of product development.
Non-clinical studies should be performed in relevant species. Considering the nature of these products this is specifically challenging. It is always recommended to seek the advice of the relevant authorities when selecting the species for non-clinical studies, especially pivotal safety studies. Homologous products could be used, however in such cases bridging data to the human product is of the utmost importance.
ATMPs and cell-based ATMPs in particular present additional challenges that should be addressed, such as:
- Cell survival status following delivery
- Cell migration or trafficking to non-target sites
- Cell differentiation into undesired cell types
- Development of an immune response to the cells
- Uncontrolled proliferation or tumorigenicity
The EMA has a set of scientific guidelines on the non-clinical testing of a medicinal product; these guidelines are provided for:
ATMPs differ from traditional medicinal products and some aspects of the guidelines may not be applicable. However, in such cases a rationale and risk assessment for not following the guidelines shall be available.
Clinical
FIRST-IN-HUMAN
When the IMP is being tested for the first time in humans, it is useful to read the following guidelines from the EMA:
- Strategies to identify and mitigate risks for first-in-human and early clinical trials with investigational medicinal products(PDF)
- Guideline on requirements for first-in-human clinical trials for potential high-risk medicinal products
PHASE I/II TRIAL OBJECTIVES
The main purpose of a Phase I/II trial is safety evaluation; this includes assessment of the nature and frequency of potential adverse reactions and an estimation of the relationship to dose (if applicable), but also other issues, such as feasibility of administration and pharmacological activity. Since the TEP candidate may in fact have little or no toxicity, other endpoints such as time to relapse, rejection and infections may be more useful. Clinical efficacy endpoints, as defined in specific guidance for the studied indication or disease, form the basis for the clinical evaluation of TEPs. Additional cell- and tissue-specific endpoints may be required such as biochemical, morphological, structural and functional parameters, which are relevant for the targeted therapeutic claim. These endpoints can be used as co-primary or secondary variables and are expected to support the clinical primary efficacy variable. Examples of endpoints should be related to conditions treated.
The tissue functionality and structural aspects of the regenerated, repaired and/or replaced tissue as well as its persistence in the human body are specific attributes of TEPs that should be considered when choosing the clinical endpoints.
FEASIBILITY ASSESSMENTS
Feasibility assessments are carried out if specialised devices or novel procedures are required for administration, customised preparation of products, special handling of products (e.g. very short expiration time) or adjunctive therapy. Consideration should be given to designing early-phase trials to identify and characterise any technical or logistical issues in the manufacturing or administration of the product. Such issues may need to be addressed before proceeding with further product development.
DOSE EXPLORATION
To the extent possible, the dose selection (i.e. cell density or concentration of main constituents) should be based on findings from quality and non-clinical product development. Dose finding studies in the clinical setting should be conducted where feasible. However, the risks relating to high or suboptimal cell numbers should be considered and addressed. Limitations of the available amount of cells/tissue in the TEP (e.g. due to autologous donation, manufacturing procedure) may lead to the use of variable doses on comparable sizes of defects. In these cases, the variable dosing should be justified and the correlation of the dose with the clinical efficacy should be carefully recorded and reported.
PHASE III TRIAL OBJECTIVES
Phase III usually is considered to begin with the initiation of studies in which the primary
objective is to demonstrate or confirm therapeutic benefit. Studies in Phase III are designed to confirm the preliminary evidence accumulated in Phase II that a drug is safe and effective for use in the intended indication and recipient population. The investigational medical product must be in a final stage. These studies are intended to provide an adequate basis for marketing approval.
IMPORTANT LINK:
Clinical aspects relating to tissue engineered products: Reflection paper EMA/CAT/573420/2009(PDF)
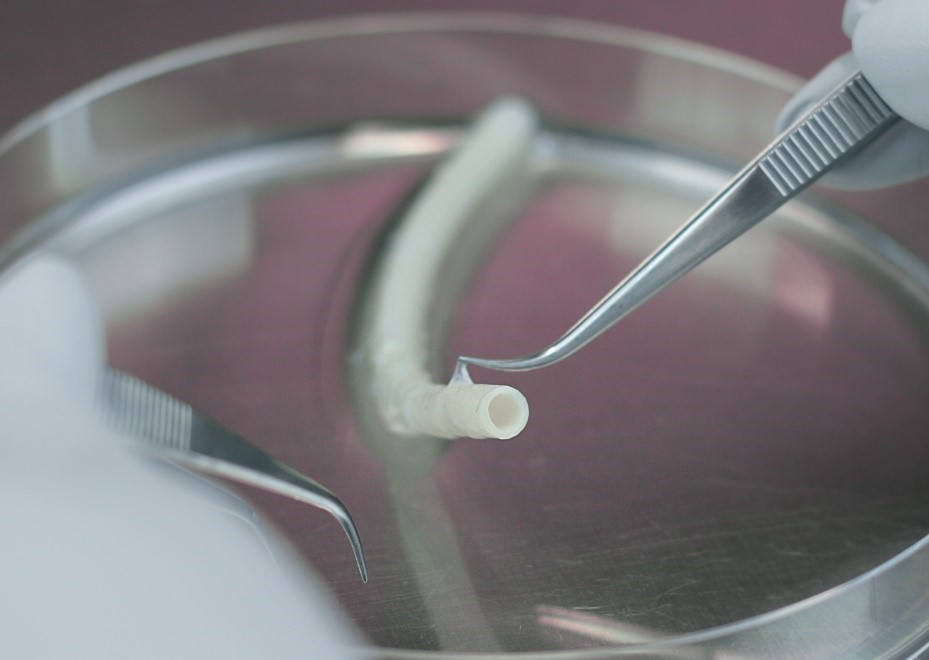
Photo by: VERIGRAFT
